In honor of the IGB's anniversary, we're revisiting some of the history of our institute over the past 15 years with a series of articles highlighting IGB people, projects, and research.
Figuring out which drugs can help cure cancer is a laborious process, often requiring decades of careful research and multiple phases of clinical trials. To this end, the “Anticancer Discovery from Pets to People” research theme at the IGB has painstakingly worked on getting two drugs into clinical trials: PAC-1 and ErSO to treat brain and breast cancer respectively. PAC-1 is currently in phase I clinical trials in humans and has been granted orphan drug status by the U.S. Food and Drug Administration for the treatment of glioblastoma, a deadly brain cancer. ErSO has been licensed by the pharmaceutical company Bayer AG and is currently being tested for human clinical trials.
One of the first steps in drug design includes testing them on animals that serve as a proxy for humans. Although researchers tested ErSO in mice models, they used a different animal for PAC-1: dogs with certain naturally occurring cancers. According to Timothy Fan (ACPP/CGD), a professor of veterinary clinical medicine, dogs may be better than rodents in many cancer drug-testing models because the latter need to be implanted with human cancer cells to mimic specific types of tumors. Additionally, certain cancers in dogs are genetically similar to those in humans and respond to the same medications. Dogs are also more similar in size to humans and are, therefore, better models to test how well the drugs work on larger tumors.
Researchers discovered PAC-1’s anti-cancer capabilities in 2006 in the Hergenrother lab. “One of the unusual features of this drug is that unlike most cancer drugs, PAC-1 gets into the brain. We wanted to embrace that and try to address the unmet clinical need of brain cancer,” said Paul Hergenrother (ACPP leader/MMG), a professor of chemistry.
PAC-1 activates the cellular enzyme procaspase-3, which triggers a series of reactions that causes only cancer cells to self-destruct, sparing healthy cells. “Even though they have elevated levels of procaspase-3, cancer cells never turn the enzyme on. They keep growing and become tumors,” Hergenrother said. “PAC-1 restores the enzyme activity and because it is elevated in cancer cells, it targets cancer cells over non-cancerous cells.”
In 2013, a $4 million investment, informed by the trials in dogs, helped PAC-1 on the road to human clinical trials. In 2016, the same anonymous donor contributed $7 million to help the studies progress in the drug-approval pipeline. Moreover, the funding also helped many veterinary patients that would not have received treatments for their cancer. PAC-1 is still in clinical trials in dogs with osteosarcoma, the most common type of bone cancer.
Fan and his colleagues are also looking at PAC-1 in combination with radiation and in combination with temozolomide, a brain cancer drug used in humans and dogs. “One of PAC-1’s greatest strengths is that it synergizes with other drugs, increasing the anti-cancer effects of many compounds that are out there,” Fan said. The three dogs in the trial tolerated the combination treatment well and responded well to the therapy. Fan said that a much larger study will be needed to quantify how much PAC-1 contributed to the positive results.
Currently in the human trials, PAC-1 has been cleared for use in a clinical trial of patients with anaplastic astrocytoma, a rare malignant brain tumor, and glioblastoma multiforme, an aggressive late-stage cancer of the brain. So far, there have been no significant side effects. The phase I trial will also determine if PAC-1 can be used safely with temozolomide. “We’ve been at this now for more than 10 years, and we’re excited to be able to continue down this road,” Hergenrother said. “It takes a lot of time, effort, and money to do human clinical trials. To expand access to PAC-1 from a dozen patients to, we hope, hundreds, is very exciting. That will allow us to get some definitive data on the drug.”
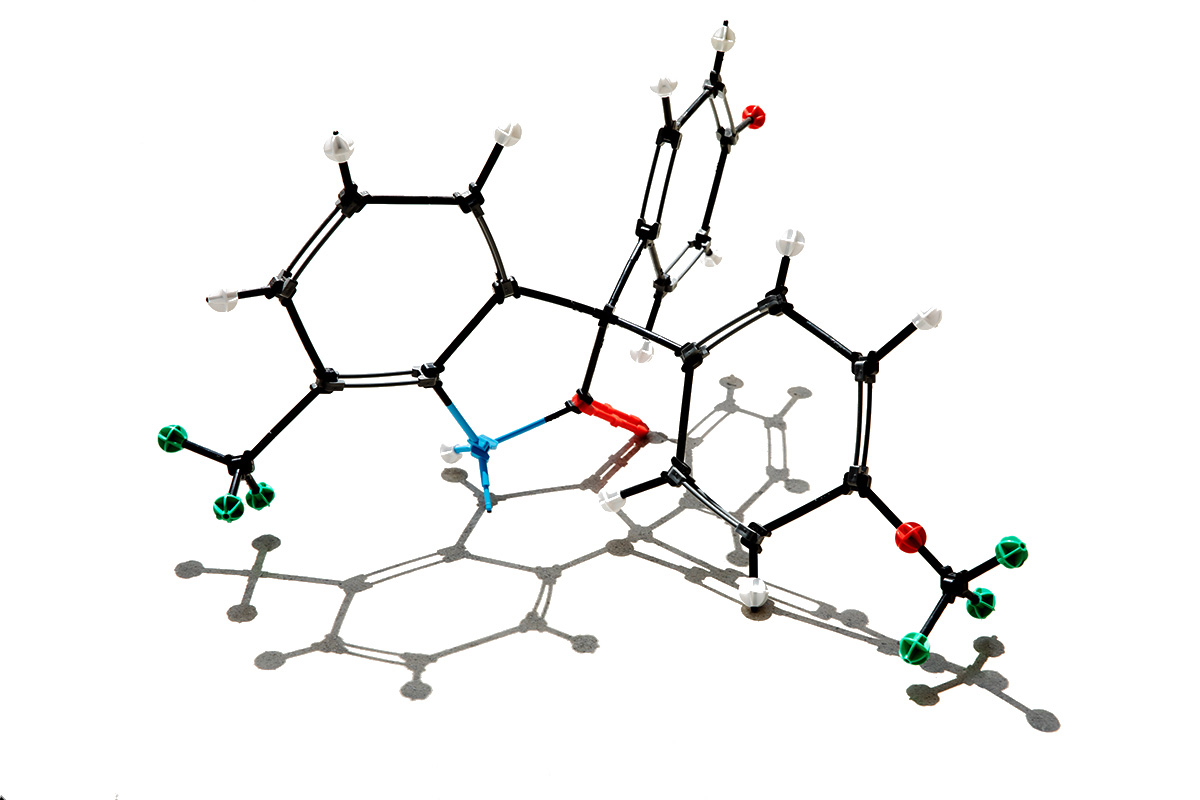
The precursor to ErSO was first discovered in 2014 in the laboratories of Hergenrother and biochemistry professor David Shapiro. Although the original compound prevented breast cancer cells from growing, it did not rapidly kill them and had undesirable side effects. In 2021, the researchers discovered the small molecule ErSO that had powerful anticancer effects without side effects in mice. When they tested the drug in mice models of human estrogen-receptor-positive breast cancers and their metastases in the bone, brain, liver, and lungs, the drug killed 95-100% of the cancer cells and shrank large tumors to undetectable levels. The compound was also well tolerated in mice, rats, and dogs.
ErSO works by binding to the estrogen receptor, upregulating the anticipatory Unfolded Protein Response or a-UPR, which kills cancer cells. About 75% of breast cancers are estrogen-receptor positive, making ErSO a potent drug. “Since the process is estrogen-receptor dependent, ErSO doesn’t touch the cells that lack the receptor, and it also doesn’t affect healthy cells—whether or not they have an estrogen receptor,” Hergenrother said.
Impressively, within a week of exposure to ErSO, advanced, human-derived breast cancers in mice shrank to undetectable levels. “Many of these breast cancers shrunk by more than 99% in just three days,” Shapiro said. “ErSO is fast-acting and its effects on breast cancers in mice are large and dramatic.”
In the past 250 years, researchers have made several discoveries that have helped in the battle against cancer, a disease that has been afflicting humanity for thousands of years. Unfortunately, patients with metastatic estrogen-receptor-positive breast cancers or glioblastoma eventually succumb to the disease, even with treatment. Although PAC-1 and ErSO may not be the silver bullet we are looking for, the studies so far have all pointed to a favorable outcome. Hopefully, as we learn more about these drugs, we will get closer to finding better weapons that can help us treat cancer.

