Gene mutation leads to epileptic encephalopathy symptoms, neuron death in mice
Mice with a genetic mutation that’s been observed in patients with epileptic encephalopathy, a severe form of congenital epilepsy, exhibit not only the seizure, developmental and behavioral symptoms of the disorder, but also neural degeneration and inflammation in the brain, University of Illinois Urbana-Champaign researchers found in a new study. The findings highlight the mutation as an important part of the disease’s pathology and a potential target for treatment.
Patients with epileptic encephalopathy begin having seizures when they are born, and display progressive developmental delay, intellectual disability and autismlike behavior, said study leader Hee Jung Chung (M-CELS), a professor of molecular and integrative physiology.
“The dogma regarding epileptic encephalopathy has been that the epileptic seizures are driving the pathogenesis of intellectual disability and developmental delay. But we wanted to answer the question, is it really just the seizures driving the intellectual disability and developmental delay?” Chung said. “This study is the first to show that expressing this human epileptic encephalopathy mutation in mice can cause not only spontaneous seizure and intellectual disability, but also neural degeneration.”
Previous work from Chung’s group found that epileptic encephalopathy is correlated with a mutation in a gene that codes for a potassium channel essential to regulating neuron activity. The mutation prevented the potassium channel from properly embedding in the cell membranes of neurons, causing it to build up inside the neuronal cells instead. Yet, whether and how the mutation played a role in the pathology of epileptic encephalopathy remained unknown.
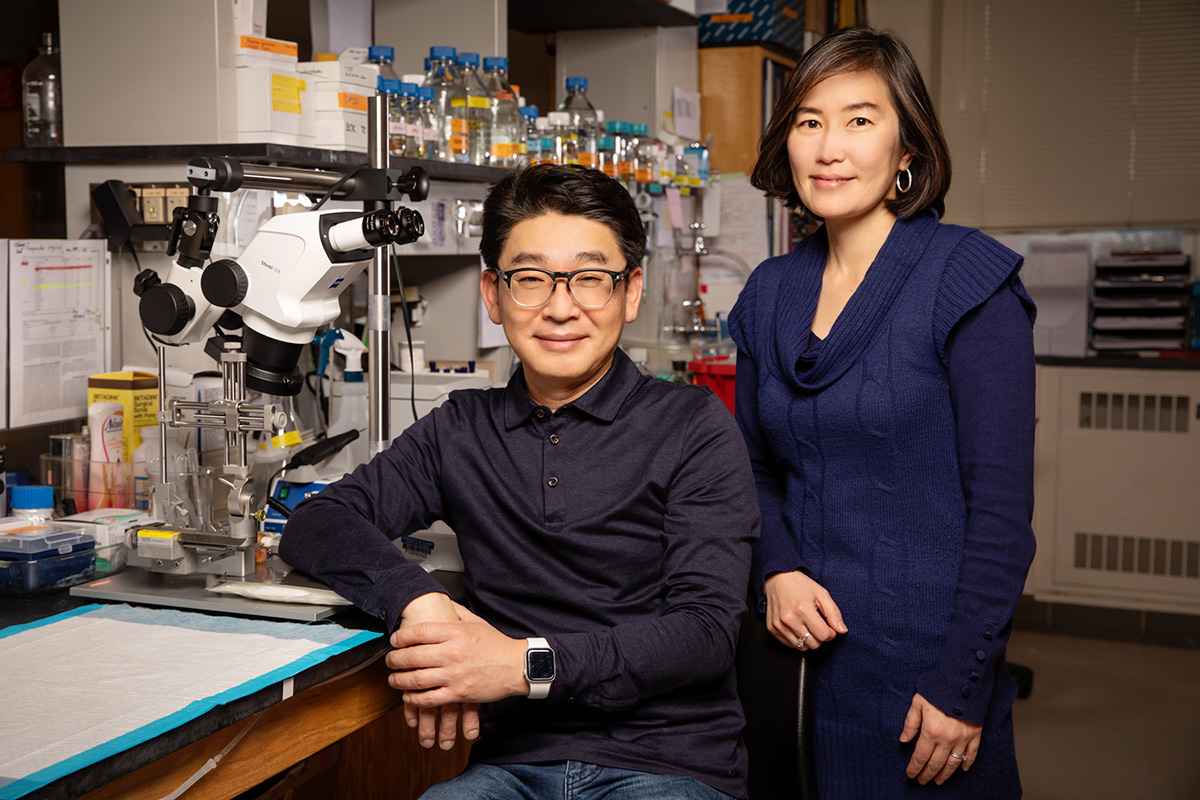
In the new study, published in the Proceedings of the National Academy of Sciences, Chung’s group, in collaboration with psychology professor Justin Rhodes (GNDP) and molecular and integrative physiology professors Eric Bolton and Catherine Christian-Hinman, bred a population of mice with the gene mutation. The researchers studied the mice from birth to observe whether they developed symptoms and how the mutation affected the expression of the potassium channels as well as their brains.
The mice developed spontaneous seizures analogous to human patients, who begin having seizures as infants. The mice also had an increase in mortality – half of mice with the mutation died as juveniles. The surviving mice showed significant deficits in learning and memory, as well as repetitive behaviors associated with human autistic behavior.
“It was very interesting to us that, from a young age, the mice displayed not only seizure activity consistent with human patients, but also the intellectual, developmental and behavioral symptoms displayed by human patients,” Chung said.
In the brain, researchers saw widespread neural degeneration and inflammation that started as early as the weaning age and grew progressively worse as the mice aged.
The findings open up two potential therapeutic targets: the defective potassium channel and the inflammation and neural degeneration, the researchers said.
“A lot of epileptic encephalopathy patients are not responsive to anti-epileptic drugs. So if we cannot block the seizures, what is the next thing to do?” Chung said. “We know that the neural degeneration is happening in mice at least as early as weaning age. Can we block that that early on before things get worse? That is a very important therapeutic intervention that we should think about.”
Next, the researchers want to study what causes the neurons to die, and whether other mutations to the potassium channel cause the same symptoms. They also hope to use the mouse line with the mutation to study potential treatments.
Postdoctoral researcher Eung Chang Kim and graduate student Jiaren Zhang were co-authors of the paper. Christian-Hinman, Chung and Rhodes are all affiliated with the Beckman Institute for Advanced Science and Technology at Illinois. The National Institutes of Health supported this work.

