Bacterial signaling across biofilm affected by surface structure
Similar to how cells within human tissues communicate and function together as a whole, bacteria are also able to communicate with each other through chemical signals, a behavior known as quorum signaling (QS). These chemical signals spread through a biofilm that colonies of bacteria form after they reach a certain density, and are used to help the colonies scavenge food, as well as defend against threats, like antibiotics.
“QS helps them to build infrastructure around them, like a city,” described Dharmesh Parmar, a postdoctoral researcher in the lab of Jonathan Sweedler (CABBI/BSD/MMG), James R. Eiszner Family Endowed Chair in the department of chemistry. “Biofilms have channels, which allow passage of nutrients, and information in the form of chemical signals. They also allow crosstalk between colonies if there's a threat or the stress in the environment.”
Biofilm formation and the subsequent resistance to antibiotics can be especially dangerous for people with a weakened immunity or with diseases like cystic fibrosis (CF), which leads to a stagnant mucus surface inside the lungs that bacteria can more easily attach to. To better understand what surface factors influence or potentially inhibit biofilm formation in the presence of antibiotics, researchers from the Sweedler lab at the University of Illinois Urbana-Champaign, along with collaborators at the University of Notre Dame, measured rate of biofilm formation via QS in a bacteria commonly acquired in hospital infections, Pseudomonas aeruginosa.
P. aeruginosa forms biofilms rapidly on a variety of surfaces, which expedites when colonies start communicating using QS, and makes treatment with antibiotics difficult. Additionally, P. aeruginosa can vary in the thickness of the biofilm it produces. The “mucoid” strain produces a thicker biofilm than the non-mucoid strain, and is often linked to infections in patients with CF, a genetic condition which increases mucus viscosity and accumulation in the lungs.
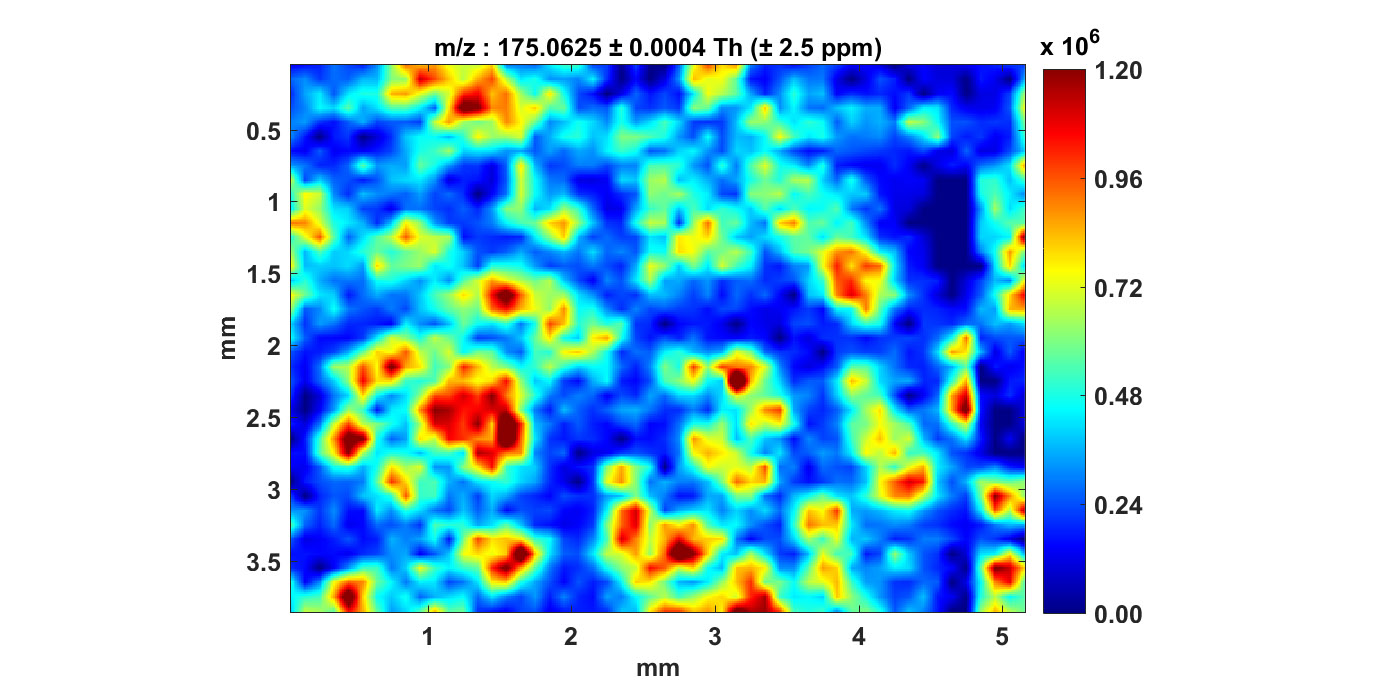
In the study, both of these strains were grown on fabricated surfaces that varied in structure, with one being uniform or “unpatterned”, and the other being “patterned” with ridged blocks. Researchers then measured how quickly colonies were able to start communicating with QS while being grown either in the presence of antibiotics or not. QS was detected using mass spectrometry and Raman-imaging, which measured the presence of signaling molecules associated with the behavior. The first thing researchers noticed was that antibiotics slowed growth of a biofilm and production of QS molecules across both strains and structure types. Next, the researchers found that surface type had a large effect on the non-mucoid strain, in that the patterned structure was associated with longer latencies before expression of QS molecules were at their peak. This was not the case for the thicker mucoid strain.
“While the impact of the antibiotic slowing biofilm growth didn’t surprise us, the large and differential impact on surface structure was striking,” said Sweedler.
“In the non-mucoid strain, surface patterning had a huge impact on the QS signal properties,” Parmar added. “In the case of mucoid, the surface structure had very minimal impact on its metabolic signatures.”
The researchers also explored how the distribution of QS signaling molecules differed across different parts of the biofilm when grown on a flat surface and exposed to antibiotics. Samples were taken from the “static biofilm”, where the biofilm attaches to the surface, the “supernatant”, or liquid medium of the culture, and the “pellicle biofilm”, that forms on top of the liquid medium and interacts with the air.
Researchers found that the supernatant liquid and pellicle biofilms contained signaling molecules associated with a stress response, while the static biofilm did not contain these molecules. The researchers think this is because the liquid component of the biofilm is what allows bacteria to float along and start new colonies elsewhere, but in the process the bacteria are also exposed to threatening situations, such as presence of antibiotics.
By comparing QS behavior during biofilm growth across these different treatments, researchers can better understand how and what kind of molecules this species of bacteria use, and gain new insights on bacterial growth.
“P. aeruginosa biofilm is quite challenging to eradicate using currently available antibiotics, and so our goal with this study was to understand what are the factors that govern the growth and stability of these biofilms, and how bacteria escapes these biofilm structures to colonize new locations,” explained Parmar.
“The chemically information-rich approaches and analytical techniques we used allowed us to probe these complex molecular events related to biofilm formation across space and time.” Sweedler explained.
The team says the next step is to use these optimized analytical techniques to measure QS signals on lung slices from rats, instead of fabricated structures like those used in the current study. Because P. aeruginosa is often associated with infections in the lungs of CF patients, understanding how it forms biofilms in the lungs can help scientists engineer methods to slow or prevent bacteria growth in these patients. Parmar described one potential future application could be to engineer surfaces of medical devices to deter bacterial adhesion and biofilm formation. These findings could also be used to help prevent biofouling, which is when bacteria spoils or degrades biological products and surfaces.
The paper is published in ACS Infectious Diseases and can be found at https://doi.org/10.1021/acsinfecdis.2c00519

