New NIH-funded research aims to improve prostate cancer outcomes
University of Illinois at Urbana-Champaign researchers recently received a $1.8 million grant from the National Institutes of Health (NIH) to develop a new assay technology that could determine the effectiveness of cancer drug treatments and aid in disease prognosis. Led by Illinois Bioengineering Assistant Professor Andrew Smith, the team is focusing on detecting nucleic acid-based biomarkers in a single drop of a cancer patient's blood.
"Very few types of cancer can be detected or monitored using bodily fluids," noted Smith. "Instead, most cancers require invasive biopsies or imaging tests that cannot monitor changes in real time."
One such example is prostate cancer, which relies on a 1970s-era blood test—the prostate-specific antigen (PSA)—to screen for the disease. If a patient's PSA level is high, he has to undergo an invasive and painful biopsy to determine whether cancer is present or not.
These conventional biopsies are unable to distinguish between slow-growing tumors that may never cause the patient harm and more aggressive forms of the disease. As a result, some patients opt for radical treatments that may be unnecessary and could compromise their quality of life.
In addition, once a patient begins drug or radiation therapy it's difficult to monitor the effectiveness of the treatment. So, Smith and his team, which includes researchers from the Medical College of Wisconsin and the Mayo Clinic, are taking an entirely different approach. By frequently measuring the concentrations of microRNA biomarkers in a patient's blood during his cancer treatments, they believe they can determine precise therapeutic regimens for each patient.
"Early data on blood-based nucleic acids such as mRNA, microRNA, and DNA suggest that these may be a highly accurate indication of a patient's cancer that can allow rapid, non-invasive, and routine analysis to measure recurrence, spread, and therapy response," said Smith, part of the IGB's Omics Nanotechnology for Cancer Precision Medicine theme and a faculty member at the Micro + Nanotechnology Lab.
According to Smith, the assay technology they are developing will be the first to read out nucleic acids from a single drop of blood. "Numerous technologies exist to measure the levels of nucleic acids—for example PCR, gene arrays, and sequencing—but none match the major challenges presented by single blood-droplet analysis needed for this clinical practice to succeed," said Smith.
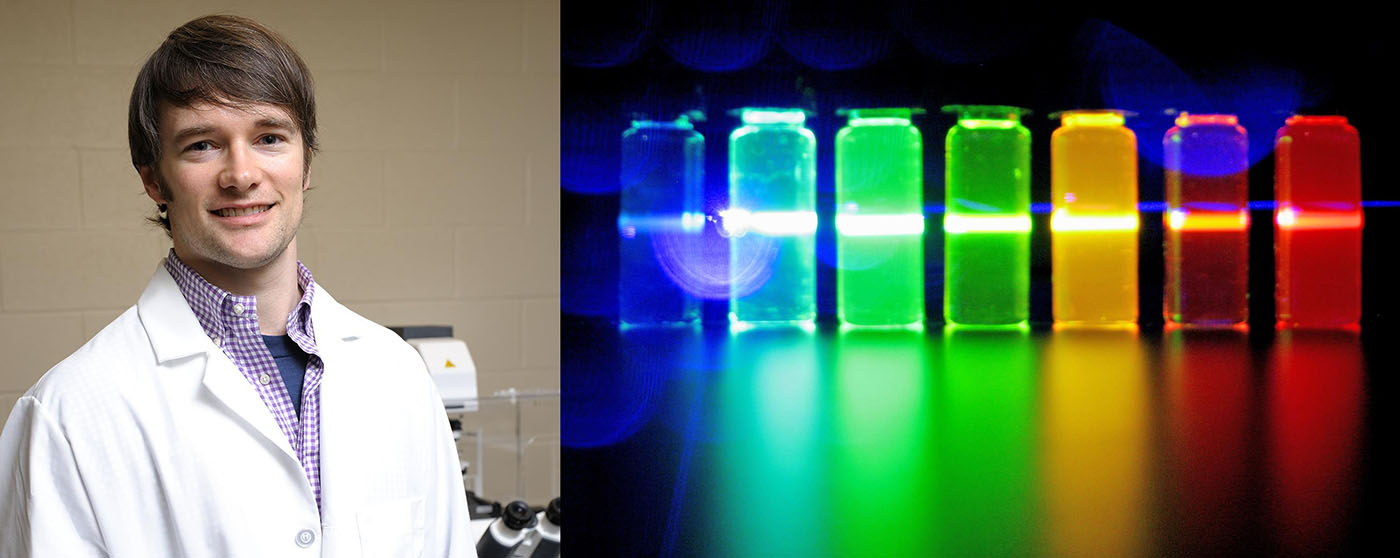
Smith's team is able to measure the nucleic acids in such a small blood sample because they know how to amplify signals from a single molecule using light-emitting quantum dots and electric field-enhancing photonic crystals.
Specifically, Smith and members of his lab (Lucas Smith and Yang Liu) are developing single-molecule optical tests for blood nucleic acids. Fellow Bioengineering faculty member Brian Cunningham, who is also an electrical and computer engineering professor, will adapt the test to mobile detection platforms that will allow patients to test their own blood at home.
The team will test its assay technology in a trial involving 100 patients with metastatic prostate cancer from the Mayo Clinic in Rochester, Minnesota. Patients will use the assay tool to draw a single drop of their own blood at home and the researchers will then use these samples to predict how individual patients will respond to prescribed cancer treatments.
Mayo Clinic oncologist and team member Manish Kohli will lead this portion of the research study. In addition, he will conduct retrospective analysis on a large repository of prostate cancer patient blood samples.
Other collaborators on the project include Liang Wang, a professor of pathology at the Medical College of Wisconsin and Rebecca Smith, an assistant professor of epidemiology at the Illinois College of Veterinary Medicine.
"If our study is successful over the next five years, our novel technology will fill a major clinical gap in knowledge, essentially allowing us to match and finely tune prostate cancer treatments to individual molecular profiles," said Smith.
