New insights into how epilancin 15X kills bacteria
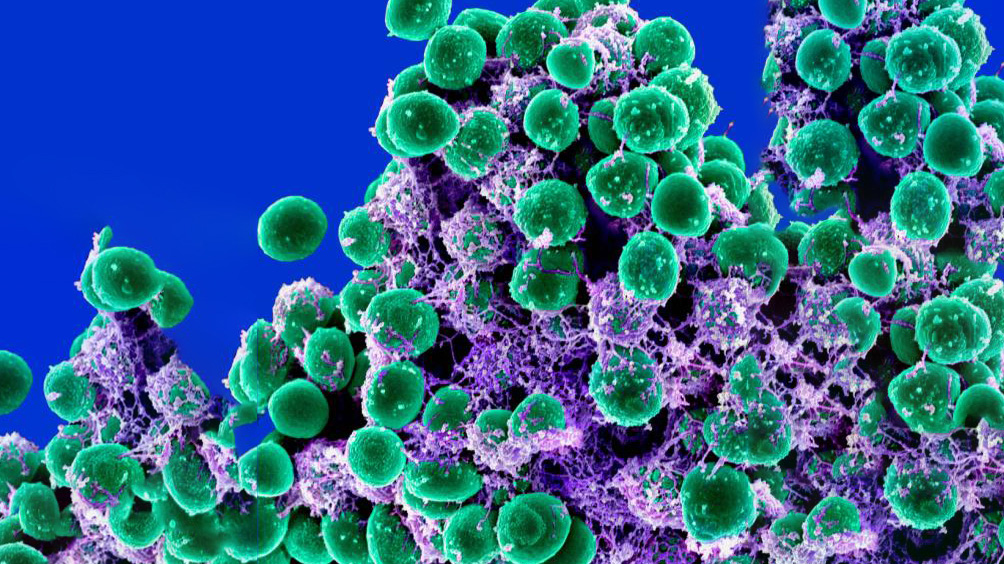
Scanning electron micrograph of a clump of Staphylococcus epidermidis (green) in the extracellular matrix, which connects cells and tissue. / National Institute of Allergy and Infectious Diseases
Antimicrobial resistance has emerged as a global threat that requires urgent attention. In a new study, published in Frontiers in Microbiology, researchers investigated how the antibiotic epilancin 15X kills bacteria.
Over the past few decades, bacteria have increasingly been able to mutate, allowing them to resist the effect of antibiotics. Coupled with the fact that antibiotics are hard to develop, this situation can soon prove to be catastrophic.
“Even after the pandemic, the industry and the government have not realized how important it is to focus on infectious diseases and antibiotic development,” said Wilfred van der Donk (MMG), a Richard E. Heckert Endowed Chair in Chemistry. “It is a sad reality that the next pandemic could be around the corner and it could be caused by bacteria.”
Over the past decade, researchers across the world and at the Carl R. Woese Institute for Genomic Biology have focused on a class of natural products called ribosomally synthesized and post-translationally modified peptides. Among these compounds, lantibiotics have emerged as promising drugs.
In the 1990s, researchers discovered the lantibiotic epilancin in a patient who had been infected by Staphylococcus epidermidis. Although these bacteria are commonly found on our skin, it can cause infections in immunocompromised patients.
“Epilancin is intriguing because it is highly active against other Staphylococci, including methicillin-resistant Staphylococcus aureus, or MRSA,” van der Donk said. “We wanted to understand why.”
The lab hypothesized that the positive charges on epilancin might be recognizing a target on the negatively charged bacterial membranes. They thought that epilancin might behave similarly to another antibiotic called nisin.
“Nisin is commercially used in the food industry to kill pathogens. If you compare the structure of epilancin and nisin, you will notice that they are largely similar,” van der Donk said. “The only difference is nisin has two rings that bind to lipid II, and these rings are different from what epilancin has.”
The researchers first tested to see whether epilancin could interfere with lipid II. To do so, they used the bacteria Bacillus subtilis that can respond to molecules that interfere with lipid II. The molecules in question are put on to a disk and if they can interfere, the bacterial colonies turn blue. They found that when the bacteria were exposed to epilancin, they did not turn blue.
The researchers confirmed their findings using artificial vesicles, which are thin sacs, that contained fluorescent molecules inside them and were covered with lipid II on the outside. “Our hypothesis was that if epilancin targets lipid II and creates a pore, then the fluorescence would change,” van der Donk said. “It did not.”
The final nail in the coffin for their hypothesis was when they compared epilancin to other antibiotics to see what cellular processes it could interfere with. To their surprise, epilancin affected the synthesis of DNA, RNA, protein, and fatty acids, but unlike nisin it had no effect on cell walls.
The group is now interested in figuring out what epilancin interacts with. “We will be looking at bacterial mutants that can resist the effects of epilancin and try to figure out what the targets are,” van der Donk said.
The study “Investigation into the mechanism of action of the antimicrobial peptide epilancin 15X” can be found at 10.3389/fmicb.2023.1247222.

