Neighborhood, breast cancer rates in African-American women linked
Neighborhood characteristics such as racial composition and poverty rates are associated with increased risks of late-stage breast cancer diagnoses and higher mortality rates among urban black women, a new analysis of recent breast cancer research shows.
Even African-American women living in low-income neighborhoods that are undergoing gentrification and economic improvement may be at significantly greater risk of having distant metastases at the time they are diagnosed with breast cancer, said lead author Brandi Patrice Smith, a graduate student in food science and human nutrition at the University of Illinois.
“This is enlightening, because an increase in overall neighborhood socioeconomic status should result in better health for residents, not worse health,” Smith said. “But because these neighborhoods were still low-income, they didn’t have as many resources,” such as health care facilities and access to mammography and follow-up care.
The study, which was published recently in the journal Hormones and Cancer, comprised a sample of more than 93,600 black women living in various large cities and urban areas across the U.S.
The dataset included patient information from state breast cancer registries in California, Georgia, Illinois, New York, North Carolina and Texas. Patients who ranged in age from 19 to 91 were tracked for an average of eight years.
Despite thousands of studies on breast cancer that have shown racial disparities in diagnosis and survival rates, only a small number of researchers have explored how these disparities might be related to various factors in women’s living environments, Smith said.
Nearly half of African-American women in the U.S. live in urban areas and about 25 percent reside in low-income neighborhoods, according to the study.
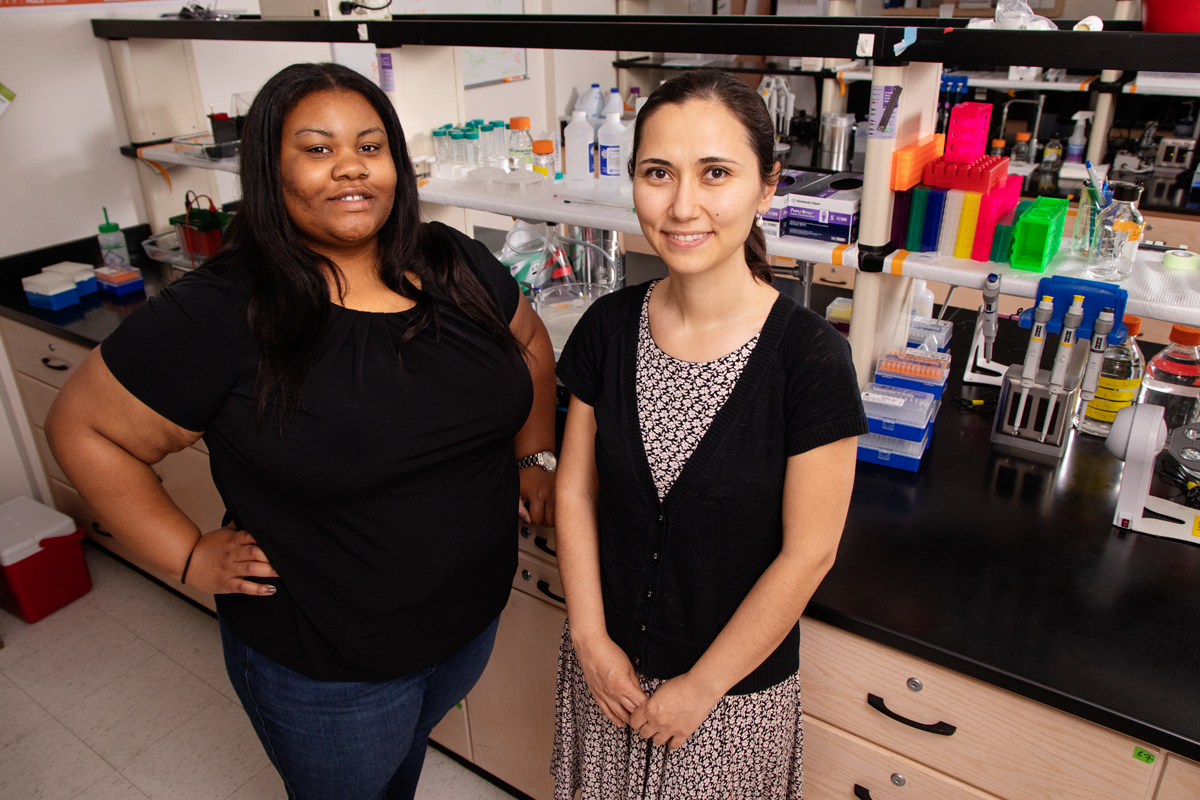
Smith and co-author Zeynep Madak-Erdogan, a professor in the same department and a member of the IGB's Omics Nanotechnology for Cancer Precision Medicine research theme, conducted a systematic review of recent breast cancer research to explore possible associations between characteristics of urban neighborhoods and breast cancer rates among African-American women. Among the factors they examined were neighborhood racial composition/segregation, poverty rates and access to mammography.
Residential segregation – which was defined as living in a neighborhood with a predominantly African-American population – significantly increased African-American women’s rates of late-stage diagnosis and doubled their chances of dying from breast cancer, the analysis showed.
Comparable mortality rates were found among white women who also lived in predominantly African-American neighborhoods, the researchers found.
“This suggests that the environmental conditions associated with low-income neighborhoods – rather than race itself – increases women’s risks of dying from breast cancer,” Smith said.
Mortality rates and risks of late-stage diagnosis were significantly greater in low-income neighborhoods where women of any race had limited access to mammograms and follow-up care with physicians, Smith said.
